Cannabis and Atherosclerosis
Cannabis and Atherosclerosis. How can cannabis contribute to alleviate atherosclerosis?
Nowadays the composition of the cannabis plant is quite well characterized. Among the different cannabinoids present within the cannabis plant those that are able to mimic the effects of endocannabinoids, that is, cannabinoids produced by our body, have raised the higher interest among scientists as they have the potential of being used to treat diverse pathologies. In particular, CBD and THC are the most studied.
Their function occurs mainly through the activation of cannabinoid receptors (CB1 and CB2) which trigger a cascade of signals inside the cell ultimately inducing, among other things, relaxation and a pleasant feeling, as well as anti-inflammatory effects, etc. this is the first link on Cannabis and Atherosclerosis.
It is well-known that the activation of CB1 receptors is usually responsible for the psychomodulatory effects of cannabis and, hence, they are mostly located in the brain, while the activation of CB2 receptors, mostly found in other tissues, is associated with effects on inflammation and pain, among other things.
There are several scientific studies on Cannabis and Atherosclerosis that show an association as well as the critical role of the endocannabinoid system with the onset and the development of this disease. It is also well known that blocking CB1 receptors plays a role in weight loss and “cardiometabolic” effects, not only in rodents but also in humans.
In addition, the effects of cannabinoids on key parameters of the cardiovascular system, such as blood pressure, vasomotor control, cardiac contractibility, vascular inflammation and angiogenesis are also well characterized.
Although endocannabinoids were initially detected in the brain and the intestinal tract, nowadays it has been shown that they are synthesized in almost every cellular type, including vascular and cardiac cells, monocytes and platelets. Furthermore, several pathologies have been associated with a malfunction of the cannabinoid system, such as some cardiac pathologies like coronary circulatory dysfunction, myocardial infarction, hypertension, atherosclerosis and diseases related to vascular dysfunction, such as diabetes, cirrhosis or obesity. In all of them, the levels of either the endocannabinoids or their receptors are altered.
It has also been shown that the endocannabinoid system has effects on the immune system, endothelial cells, the metabolism of lipids and also on smooth muscle cells, all of which are key players in atherosclerosis.
Cannabis and Atherosclerosis, effects on the immune system:
Cannabinoids, through their CB1 and CB2 receptors, are able to modulate and regulate the immune system. Since inflammation plays an essential role in this pathology, it is important to understand the contribution of cannabinoid-mediated modulation.
A groundbreaking study on an animal model of atherosclerosis showed that the oral administration of low THC doses (1 mg/KG/day) inhibited the progression of atherosclerotic lesions. THC reduced the adhesion of immune cells (such as macrophages) and their recruitment into the space located between blood vessels and tissues (the subendothelial space) through the activation of CB2 receptors. It was also shown that THC reduced the expression of proteins involved in the recruitment of immune cells (known as cytokines) and, in particular, those that recruited lymphocytes (mainly TH1, the most abundant cells in atherosclerotic lesions). What made this model unique was that the dose used to treat such lesion was way lower than that required to trigger the psychotropic effect of THC.
Similar results were observed in other animal models using synthetic cannabinoids such as WIN55212-2. In all studies the beneficial effect of the treatment was associated with the anti-inflammatory effect of cannabinoids.
The effects mediated by CB1 receptors were corroborated in cell cultures with human immune system cells. In addition, a substantial increase in CB1 receptors was also observed in biopsies taken from patients suffering from different types of angina.
Effects on the endothelial cells:
Dysfunction (malfunction) of cells from the vascular endothelium (cells lining the blood vessels) plays an important role in the pathogenesis and complications of atherosclerosis.
The presence of CB1 receptors has been shown in cells from the aortic endothelium in humans. It has also been shown that blocking this receptor can inhibit the harmful effects on endothelial cells.
Likewise, it has also been shown that the activation of CB2 receptors in endothelial cells reduces inflammation as well as the expression of adhesion molecules such as VCAM, that are essential for the infiltration of immune cells into the subendothelial space.
Effects on the metabolism of lipids:
The oxidation of lipids (fat) plays a main role in the pathogenesis of atherosclerosis. It has been shown that CBD has the ability to inhibit the oxidation of LDL (which would originate ox_LDL) and, hence, it could be used to prevent the progression of atherosclerosis, since ox_LDL accumulates in the wall of arteries causing an atheroma.
It has been shown that ox_LDL is able to potentiate the endocannabinoid system in macrophages (cells from the immune system). Such effect is associated with an increase in the amount of lipids within macrophages.
Furthermore, the endocannabinoid system is able to modulate the lipid pattern of the organism, so it might have an essential role in the progression of this pathology.
Effects on smooth muscle cells:
There are contradictory reports regarding the role of CB1 and CB2 receptors and their involvement in the growth of smooth muscle cells. While CB1 mediated pathways have a “pro” atherosclerotic effect, CB2 pathways seem to protect against this pathology by modulating and promoting a better functioning of the vascular endothelium.
Although CBD and THC are the two best-studied compounds, there is another substance present in plants that is also gaining importance, a terpene known as caryophyllene (present in plants such as rosemary, clove, etc.).
More recently, it has been shown that the administration of caryophyllene inhibited the infiltration of macrophages into the aorta and, in turn, reduced the blood concentration of cholesterol and triglycerides. This study suggests that caryophyllene could also be able to prevent Alzheimer’s disease.
A parallel study also showed that caryophyllene binds to and activates CB2 receptors, reducing inflammatory responses.
Increased oxidative stress (accumulation of free oxygen radicals) can cause the oxidation of LDL and their subsequent accumulation. Such oxygen radicals are targeted by the immune system since they damage organs and tissues.
It has been suggested that CBD, through the activation of the endocannabinoid system, might become a therapeutic option against oxidative stress. In addition, the antioxidative effect of CBD might protect us from many diseases associated with these free radicals.
What is Atherosclerosis?
We have 4 different types of lipoproteins in our blood that are used to transport fatty acids and cholesterol to our tissues and organs. These 4 types are:
1. Chylomicrons.
Chylomicrons capture fatty acids in the intestine that are of dietary origin (triacylglyceride or TAG).
2. VLDL.
Acronym for Very Low Density Lipoproteins, VLDL are responsible for capturing and transporting the fatty acids that accumulate in the liver (TAG), since an excessive accumulation of fatty acids in the liver might be unsafe (hepatic steatosis or fatty liver disease). There is a particular enzyme known as lipoprotein lipase (LPL) and found in different tissues that breaks down TAG from chylomicrons and VLDL into cholesterol and phospholipids, slightly increases their density in the process. They first become IDL (Intermediate density lipoproteins) and then LDL (low density lipoproteins).
3. LDL.
Acronym for Low Density Lipoproteins, also known as “the bad” cholesterol, see below why. They mainly transport cholesterol to the tissues through the bloodstream.
4. HDL.
Acronym for High Density Lipoprotein. Associated with the “good” cholesterol these are the “return” lipoproteins, as they absorb cholesterol from the tissues and carry it back to the liver. They literally bite the tissue membranes and carry cholesterol to the liver, scavenging the leftovers.
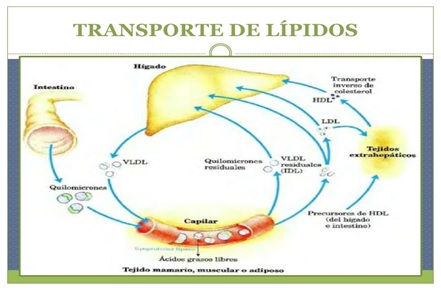
Esquerra-Dreta/Superior-Inferior
Intestine/Liver/ Reverse Cholesterol Transport/HDL
Chylomicrons/VLDL/Residual Chylomicrons/Residual VLDL (IDL)/LDL/ Extrahepatic tissues
Capillary/HDL precursors (from liver and intestine)
Free fatty acids
Mammary, muscle and adipose tissue
Picture showing the circulation of lipoproteins
Image from: https://es.slideshare.net/macr091/i-05-lipidos-lipoproteinas-y-transporte
LDLs are known as the “bad” cholesterol because an excess of cholesterol in the blood causes the oxidation of the cholesterol carried in LDL as well as their precipitation and accumulation in the walls lining the blood vessels, leading to inflammation and the recruitment of immune system cells, mainly macrophages.
Macrophages are the main phagocytic cells of the immune system (they “eat” infectious agents and unwanted particles that may cause an infection, and destroy them, while also presenting them to other cellular types of the immune system) but they eventually die during the eating and destruction process and also accumulate in the endothelial walls, causing an atheroma.
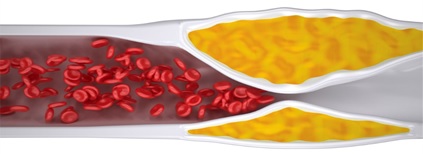
If the excess of cholesterol in blood prolongs over time, the accumulation of debris and dead cells causes a severe narrowing of the blood vessels that obstructs the blood flow and leads to atherosclerosis. The narrowing of the blood vessels is a frequent cause of cardiovascular disorders that may result in death.
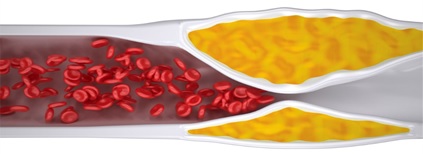
Graphic representation of the narrowing of the blood vessels and the obstruction of the blood flow (blood cells are shown in red) caused by the accumulation of dead macrophages and precipitated cholesterol (shown in yellow). Image from: https://www.health.harvard.edu/heart-health/ask-the-doctor-checking-for-blocked-arteries-in-heart-failure.
In order to reduce cholesterol it is common to use treatments based on resins and inhibitors of HMG-CoA reductase, which have two simultaneous modes of action: resins act by hindering the uptake of dietary cholesterol (only 10% cholesterol is recycled, instead of 95%) although by doing so our body will try to compensate promoting the synthesis of cholesterol in the liver. If we simultaneously inhibit the HMG-CoA reductase enzyme, we impair its synthesis as well and, therefore, the amount of available cholesterol is reduced. These treatments are mainly used to treat familial hypercholesterolemia.
Cannabis and Atherosclerosis. Analyzed and discussed by Paula Pifarré, PhD. Cannabity Healthcare Scientific Collaborator.
References
1- Sandeep Singla et al, 2012. Clinical Cardiology
2-Alexander I Bondarenko, 2019. Recent Advances in Cannabinoid Physiology and Pathology
3-https://www.projectcbd.org/es/condition/11/La-Aterosclerosis
4-https://www.cannabisreports.com/cannabis-studies/cannabis-for-atherosclerosis

 Aceite de CBD 10% de 10ML – Full Spectrum – Nacional
Aceite de CBD 10% de 10ML – Full Spectrum – Nacional 




Responses