Cannabis and Ashtma

Cannabis and Ashtma. The bronchodilator effect of Cannabis
The anti-inflammatory effect of cannabinoids has been studied since the 70s. One of the first studies on Cannabis and Ashtma tried to determine whether the use of Cannabis sativa had beneficial effects for patients with asthma.
Several studies focused on comparing the effects of THC with those of common drugs used to treat asthma, such as Isoprenaline and Salbutamol.
These studies have shown that THC has a bronchodilator effect that lasts for at least a couple of hours at an equivalent dose than that used for Isoprenaline.
When compared with Salbutamol, and although both substances improve the respiratory activity, Salbutamol acts faster but loses its effects earlier than THC.
THC has a bronchodilator effect in healthy patients as well as in patients with chronic asthmatic bronchitis by increasing the airflow and reducing bronchoconstriction.
The effects of THC are also observed when smoking marijuana, although to a lesser extent due to the irritating effect of smoke. The presence of carbon monoxide (CO) and tar in the smoke affect the respiratory system. Therefore, the most effective way to administer THC would be by using vaporizers with medicinal cannabis.

Image: http://teledoc.cl/
Cannabis and Ashtma. The anti-inflammatory effect of Cannabinoids
It has been shown that the cannabinoids present in the Cannabis sativa plant have potent anti-inflammatory and analgesic effects through the activation of the cannabinoid receptors (CB1 and CB2) located in cells of both the central nervous system (CNS) and the immune system, although cannabinoid receptors have also been found in lung tissue.
It has also been shown that CBD interacts with receptors involved in the modulation of inflammatory response as well as gene expression.
The presence of immune system cells such as T-Helper-2 lymphocytes in the lungs is closely related to the development of asthma. T-Helper-2 lymphocytes, also known as CD4+ lymphocytes, are a type of immune system cells that produce small molecules known as cytokines, mainly the interleukins IL-4, IL-5 and IL-13. These molecules act as modulators of the inflammatory response.
There is a recent study that shows how the treatment with CBD in asthmatic rats significantly reduced the cytokine levels for IL-4, IL-5, IL-13, IL-6 and interferon alpha (INF-α), which reduced the manifestation of clinical symptoms in this particular model. These results suggest that CBD might be a potential therapeutic compound for the treatment of asthma.
Cannabis and Ashtma spams
The ability of cannabis to reduce muscle spams (involuntary contractions) that occur during an asthma attack has also been investigated. The smooth muscle that lines the bronchioles contracts during an asthma attack and causes a narrowing of the airways.
There are recent studies that suggest the involvement of both receptors in the beneficial effects of cannabis on the respiratory system. It has been shown that THC negatively regulates the expression of ionic channels in epithelial cells of the respiratory tract. It has also been shown that CB1 receptors inhibit bronchospasms and, hence, have a bronchodilator effect. In addition, CB2 receptors have been shown to prevent bronchoconstriction and pulmonary edema in animal models, on top of their already known anti-inflammatory effect.
Effect on respiratory airways
It is well-known that smoking harms our respiratory system. Smoking cannabis also causes alterations in the respiratory system, inflames the airways and damages mucous glands.
When evaluating the combined and independent effects of smoking tobacco and marijuana on respiratory symptoms and chronic obstructive pulmonary disease (COPD), it has been shown that smoking marijuana does not increase the risk of COPD but it does increase the damage caused by tobacco. Consumption of both substances is, therefore, discouraged.
In conclusion, cannabis does not causes pulmonary emphysema or the narrowing of the bronchioles but it may aggravate the damaged caused by tobacco in patients that smoke both tobacco and cannabis.
What is the best way to use medicinal cannabis?
The use of cannabis on the respiratory system is highly polemic, mostly because its more common use involves smoking, but the novel modes of administration that involve aerosols and vaporizers question this myth and open new possibilities for the scientific community to keep on investigating on cannabis and the treatment of respiratory diseases.
It is important to remember that people with asthma who wish to be treated with cannabis should seek professional advice and refrain from quitting conventional treatments without proper medical counseling.
What is Asthma?
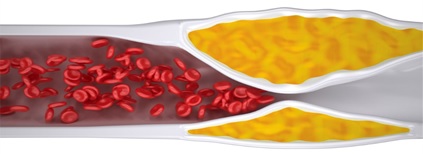
Asthma is a respiratory disease. It is characterized by the inflammation of the airways (bronchioles) due to an increased bronchoconstriction activity in response to several endogenous and exogenous stimuli.
The main symptoms are: breathing difficulty, shortness of breath (dyspnea), thoracic oppression, cough and wheezing.
During an asthmatic crisis there is an inflammation of the muscles surrounding the airways that limits the passage of air. If no action is taken, it can cause the extreme narrowing of the airways due to the accumulation of mucus that restricts even more the flow of air towards the lungs.
Asthma is a complex disease that involves three fundamental components:
- Inflammation of the airways
- Discontinuous airflow obstruction
- Bronchial hyperreactivity
Inflammation of the airways and bronchial hyperreactivity
Asthma is caused by the acute, subacute or chronic inflammation of the airways. The secretion of mucus obstructs the airways and contributes to bronchial hyperreactivity (bronchioles overreact to multiple stimuli such as allergens, contamination, tobacco, etc.).
The cells of the immune system that are involved in bronchial inflammation are: mast cells, eosinophils , epithelial cells, macrophages and T lymphocytes.
Mast cells are cells that play an important role in the immediate response to allergens, airways inflammation and hyperreactivity. They belong to the innate immune system, which constitutes the first line of defense of our organisms against pathogens and allergens. Macrophages, eosinophils and T lymphocytes are cellular types that are involved in the chronic inflammation of the respiratory system caused by bronchial hyperreactivity.
T-helper lymphocytes are classified in several groups (Th1, Th2, Th17…) and their secretion products play a central role in the inflammatory response within the airways. It has been shown that lymphocytes Th17 are involved in inflammatory asthma. The molecules released by these lymphocytes attract other cells of the immune system and increase inflammation. IL-13 has also been shown to play an important role in the production and release of histamine (increases inflammation), in bronchial hyperreactivity, and in the secretion of mucus.
The release of IgE (an antibody type exclusive of mammals that modulates allergies) takes place when our organism is exposed to antigens, such as pollen, pollen mites, air pollutants, etc. IgE binds to receptors found in cells of the immune system such as mast cells, eosinophils and basophils, and promotes the release of cytokines and proinflammatory molecules, increasing inflammation in the bronchial and alveolar areas.
Any compound able to regulate the inflammation of the airways is a potential therapeutic agent to treat this pathology.
Intermittent airflow obstruction
Bronchoconstriction takes place when the smooth muscle that lines the bronchioles contracts and reduces the airflow. This contraction occurs in response to several mediators and neurotransmitters and it is reversible to a great extent through the activity of bronchodilator drugs.
What causes Asthma?
The combination of genetic and environmental factors has been associated with asthma. Among the environmental factors involved are air pollutants, allergens such as pollen, pollen mites, or molds as well as the exposure to toxic substances such as the formaldehyde found in PVC.
Regarding the genetic factors, several studies have isolates genes or groups of genes related to asthma. As much as 25 genes have been associated with asthma and many of them are involved in the immune response, mainly in the regulation of inflammation.
Approved treatments for Asthma
Approved treatments for asthma focus on alleviating the symptoms and improving patients’ quality of life, since asthma is considered a chronic disease for which there is no definitive cure.
Two main groups of drugs are used to treat asthma:
Bronchodilators and anti-inflammatory drugs.
Anti-inflammatory drugs treat the inflammation of mucous membranes and usually consist of corticosteroids (budesonide, fluticasone, mometasone). These corticoids are administered using inhalers to ensure that they reach the affected tissue directly.
Beta-2 adrenergic receptor agonists are also used to treat asthma due to their ability to dilate the bronchioles. They are known as bronchodilators. These compounds relax the smooth muscle that lines the airways and facilitate the flow of air. Bronchodilators such as salbutamol are used during acute asthma attacks.
References
2-Bronchodilator effect of delta1-tetrahydrocannabinol administered by aerosol of asthmatic patients
3-Allergen challenge increases anandamide in bronchoalveolar fluid of patients with allergic asthma.
4-Evaluation of Serum Cytokines Levels and the Role of Cannabidiol Treatment in Animal Model of Asthma.
5-Cannabinoids inhibit cholinergic contraction in human airways through prejunctional CB1 receptors
6-Respiratory and Immunologic Consequences of Marijuana Smoking
7-Cannabis and tobacco smoke are not equally carcinogenic
8-Chang SW. et al, 2018, Biochem. Biophys. Acta Gen Sub
9-Grassin-Delyles S. et al, 2014, Br. J. Pharmacol.
10-Shang VC. et al, 2016, Biochem. Pharmacol.
11-Cui YY. et al, 2007, Eur. J. Pharmacol.
Cannabis and Ashtma. Analyzed and discussed by Paula Pifarré, PhD. Cannabity Healthcare Scientific Collaborator.

 Sérum Facial con CBD – Aceite antienvejecimiento (Cannabidiol) 30ML
Sérum Facial con CBD – Aceite antienvejecimiento (Cannabidiol) 30ML 



Responses